Hib
Key facts
-
Hib (Haemophilus influenzae type b) causes a variety of serious illnesses, including swelling around the brain (meningitis), blood poisoning (septicaemia), swelling in the throat and lung infections (pneumonia).
-
Children who get Hib infections before two years old do not usually develop natural immunity.
-
Hib-containing vaccines are the best way to protect your child from Hib.
On this page
- What is Hib?
- What will happen to my child if they catch Hib?
- What vaccine will protect my child against Hib?
- When should my child be vaccinated?
- How does the Hib vaccine work?
- How effective is the vaccine?
- Will my child catch Hib from the vaccine?
- What are the common reactions to the vaccine?
- Are there any rare and/or serious side effects to the vaccine?
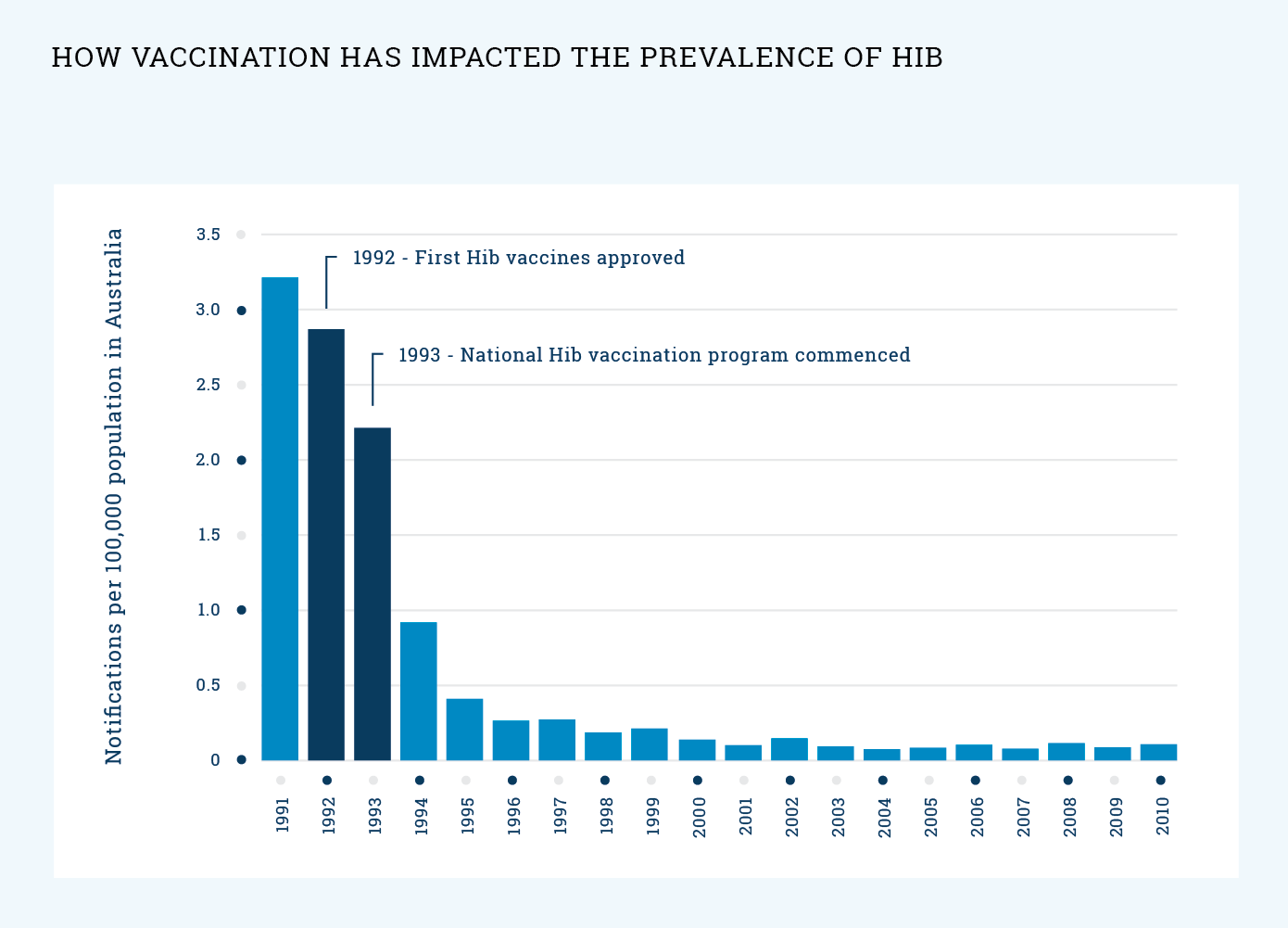
- What impact has vaccination had on the prevalence of Hib?